Issue #50 // Beyond the Blood Draw
Monitoring Blood Lactate Continuously, Non-Invasively, and In Real-Time
Liked this issue? If so, you can show your support by tapping the 🖤 in the header above. It’s a small gesture that goes a long way in helping me understand what you value and in growing this newsletter. Thanks!
Issue № 50 // Beyønd The Bløød Draw
The scientific literature is filled with evidence of biomolecules generated during exercise that may hold promise for therapeutic interventions including BDNF for Parkinson’s, lactoyl phenylalanine for diabetes, irisin for Alzheimer’s, and more. It isn’t an exaggeration to say that exercise is medicine.
Like all medicines, though, we need to understand different exercise’s dose-response relationships in order to prescribe them effectively. This is true whether you’re using exercise to stave off disease, improve athletic performance, or elicit a specific training adaptation such as skeletal muscle hypertrophy. In all cases, we need accurate and accessible ways to measure the body’s physiological responses to physical activity. I’ve spent a meaningful amount of time working on this problem over the years, and two of the biomarkers I’ve found particularly useful for physiological monitoring during exercise are muscle oxygenation (SmO2) and blood lactate, both of which are local indicators of metabolic stress in tissues1.
Measuring muscle oxygenation is relatively straightforward, and can be done with a number of commercially available sensors, including the NNOXX One. Measuring blood lactate, on the other hand, has traditionally been more challenging, requiring a blood draw from the ear or finger tip. However, recent advancements in wearable technology have opened new possibilities for non-invasive, real-time, lactate monitoring that could transform both clinical exercise interventions and high performance athletics.
Muscle oxygenation and blood lactate are fundamentally linked to the bioenergetics of muscular work. Yet, the relationship between these two biomarkers is complicated and can vary depending on relative exercise intensity and duration, carbohydrate consumption, and environmental conditions, among other factors.
Broadly speaking, though, as exercise intensity increases, muscle oxygenation decreases and blood lactate levels rise. The reason for this is simply — muscle oxygenation reflects the balance of oxygen supply and demand in exercising muscles. Past a certain level of exercise intensity, the muscles consume more oxygen than can be supplied to them, and as a result muscle oxygenation levels decline. Simultaneously, blood lactate levels increase as glycolysis provides an increasing fraction of energy to power activity.2
Thus, we should expect to see an inverse association between muscle oxygenation and blood lactate levels during exercise, particularly as intensity increases. However, this association is non-linear — muscle oxygenation and blood lactate are weakly correlated at rest and during low intensity exercise and become more strongly correlated at higher exercise intensities. In my personal experience collecting data on myself and individual I’ve tested, Pearson correlations between muscle oxygenation and blood lactate levels range from -0.66 to -0.94 depending on the intensity of exercise, with the strongest correlations occurring during moderately challenging to maximal effort exercise.
Notably, the aforementioned correlations are from un-corrected data. A major limitation with simply comparing time series muscle oxygenation and blood lactate data is that muscle oxygenation levels change instantaneously in response to increased loading whereas there’s a three to five minute time lag between when lactate is generated in tissue and when it can be measured in the systemic circulation via blood draw. When accounting for this, and correcting for it by shifting blood lactate measurements backward by three minutes the correlation between muscle oxygenation and blood lactate is significantly strengthened (r = -0.77 to -0.98).
Given the strong correlations between time-series muscle oxygenation and blood lactate data, one might assume that predicting blood lactate levels from muscle oxygenation measurements is trivial. However, while intra-individual correlations are robust— allowing for reliable predictions within a single person's data— inter-individual predictions present a more complex challenge.
The primary difficulty lies in the substantial variation in how much blood lactate levels change relative to muscle oxygenation across different individuals. Factors including age, sex, anthropometrics, body composition, training status, nutrition, and genetic factors all influence this relationship, creating significant heterogeneity in the slope and intercept of these correlations across individuals3.
Conceivably, there are a few ways to circumvent this problem, allowing for the creation of a real-time, non-invasive, blood lactate measurement. First, we can collect simultaneous muscle oxygenation and blood lactate data for a population at scale along with the relevant metadata (fitness level, body composition, age, sex, anthropometrics, etcetera) needed to derive a formula, with weights and coefficients, that can be modified based on known parameters about an individual. This would allow us to create a measure that can be used on various people without having prior knowledge about them. The second solution is to record muscle oxygenation and blood lactate data for a given individual, across a range of exercise intensities, then create a mapping between the two measurements, which would allow us to predict blood lactate levels real-time from their muscle oxygenation measurements.
Of the two solutions above, the first is then more desirable approach if the goal is to develop a consumer friendly, non-invasive and real-time, blood lactate measurement that can be easily deployed for exercise tracking. However, the obvious downside is that this approach requires time and money. While these are not impediments to a large consumer wearable company I, unfortunately, do not have the luxury to pursue this solution in my free time. The second solution, on the other hand, is easier and more practical, and is something I’ve personally done time and again. However, the downside is that it requires sufficient prior data collection which is time consuming, and uncomfortable (it requires frequent blood draws).
Between these two extremes outlined above lies a third approach. We’ve already discussed how muscle oxygenation and blood lactate are strongly correlated, but that the magnitude by which lactase changes relative to muscle oxygenation depends on a number of factors. Notably, however, when performing feature selection on reasonable sized datasets I’ve found that fitness level is one of the strongest influences on this relationship. Thus, it’s conceivable that given a relatively homogenous population (say, competitive cyclists) we can create a one-size fits all muscle oxygenation to blood lactate conversion formula that can be used "off the shelf" without prior testing. Let’s call this the pseudo individualized approach.
To test the "pseudo individualized" approach discussed in the previous section, I recruited a ~dozen competitive cyclists to collect muscle oxygenation and blood lactate data during a ramp incremental exercise test and an unstructured sixty to ninety minute ride on the road. Using this data, I found that the following second degree polynomial formula best predicted blood lactate levels given an individual’s muscle oxygenation data:
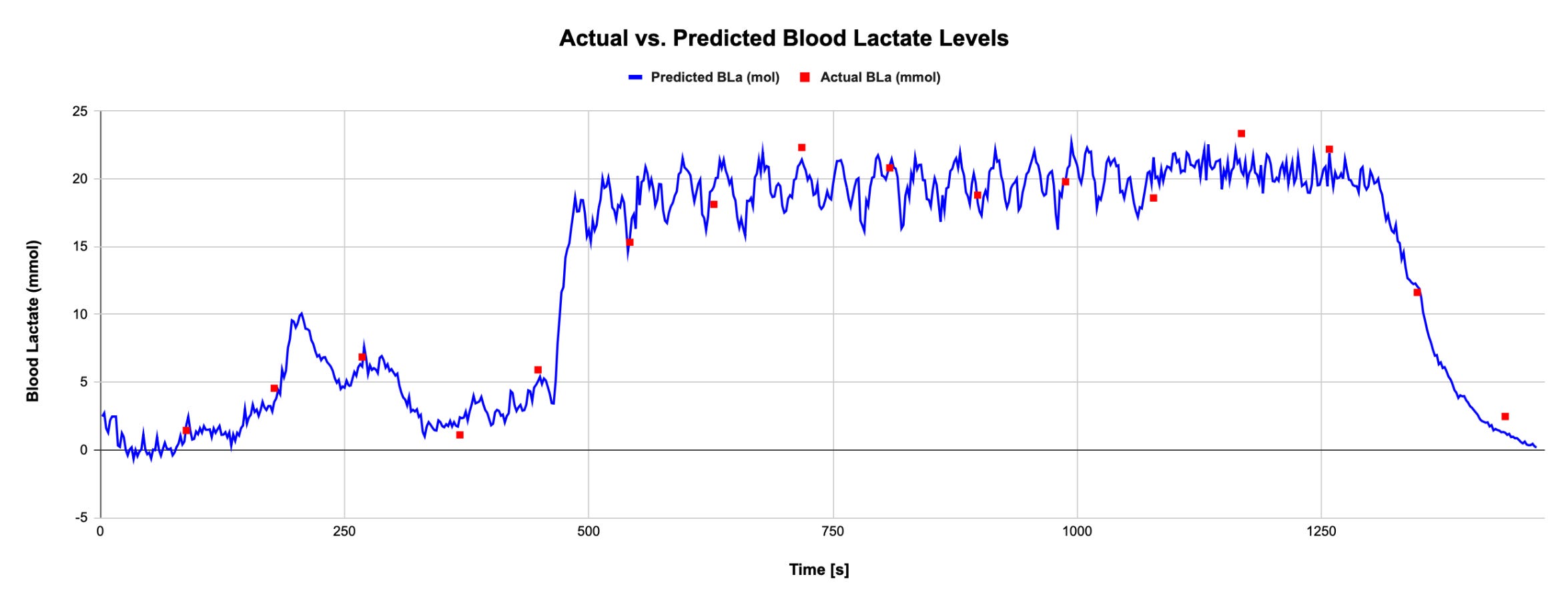
To validate the formula above in our target population I collected three other cyclist’s muscle oxygenation (SmO2) and blood lactate (BLa) data who were not part of the initial data collection used to develop the model. For each of these individuals I predicted their blood lactate levels, then compared that to their actual collected blood lactate (via blood draw) to see how accurate the model was. Below you’ll find an exemplar dataset comparing actual and predicted blood lactate levels:
Across the three test subjects mentioned above, the average RMSD for blood lactate was 1.2 mmol. So, our prediction wasn’t perfect, but it was very close, and good enough to guide training and racing, and track progress over time. Additionally, our approach pseudo individualized approach offers several advantages over traditional blood lactate testing. First of all, it doesn’t require a blood draw, which is a major plus. Secondly, it provides a real-time, continuous, measure of blood lactate levels, which is something that was never possible previously— in the lab, we’d typically measure blood lactate once every ~five minutes and out in the field the window between measurements can vary even more.
The potential applications for non-invasive, real-time, blood lactate measurements extend in several directions, independent of the approach we use to make these measurements. For example, professional sports teams and elite athletes, who already have access to advanced physiological monitoring tools, could readily implement personalized muscle oxygenation-to-blood lactate conversion formulas as part of their performance analytics toolkit.
For the broader endurance sports community (runners, cyclists, rowers, etc), specialized applications could be developed to implement the pseudo individualized approach above. These applications would leverage the homogeneous population approach, offering reasonably accurate lactate predictions without requiring individual calibration. Perhaps most excitingly, large scale data collection could be used to develop a near universal blood lactate prediction, opening the door for widespread visualization of blood lactate dynamics in real-time with unprecedented resolution.
Interested in working together? I advise small companies, startups, and VC firms on topics ranging from biosensor development, multiomics and biometric data analysis, network modeling, and product strategy. Contact eva♦peiko♦@gmail.com (replace the ♦ with n) for consulting inquiries or newsletter sponsorship opportunities.
If you’re interested in learning more about why I’ve singled out these two measurements in particular, you can check out the case study in the PhysioNexus readme. Across a number of athletes, and sports, I’ve seen muscle oxygenation and blood lactate act as central hubs- both by degree and betweenness centrality— emphasizing their importance in driving other system level physiological responses and serving at information brokers, connecting different processes.
Lactate is not a fatigue by-product, but rather an intermediate energy source in muscle metabolism. If you’re interested in learning more about this topic, see the video below.
If you’re interested in learning more about the various factors contributing to inter- and intra-individual variations in muscle oxygenation measurements you can check out my previous article titled Dampening the Noise: Making Sense of Variability In Biometric Measurements.